Understanding the Role of Embolisation in Hypervascular Tumour Treatment
Published on March 28, 2025
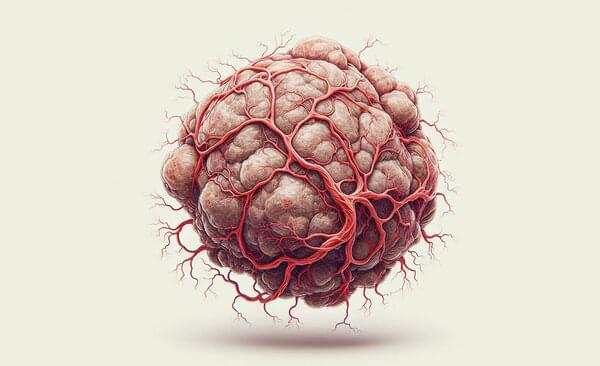
The treatment of hypervascular tumours requires careful consideration and planning by healthcare professionals due to the extensive network of blood vessels supplying these tumours. The presence of a high vascular density can complicate surgical resection, increasing the risk of excessive bleeding, prolonged operative times, and potential clinical complications. Embolisation is frequently employed as part of a comprehensive treatment strategy in these cases. This technique involves the targeted occlusion of the tumour’s blood supply to support the reduction of blood loss and assist with surgical access and excision.
Considerations and Potential Risks
The mitigation of risks when treating hypervascular structures around a tumour in any part of the body requires extensive planning and preparation. It can be difficult to distinguish between tumour and vessels, and to establish a safe resection pathway. This is why a comprehensive assessment with diagnostic imaging such as CT or MRI is crucial as part of the planning process.i Histological evaluation further aids in understanding the tumour’s behaviour and vascularisation, informing a strategic and individualised treatment approach.
Although embolisation is a well-established technique, it carries potential risks, as with any medical procedure. These may include respiratory complications, particularly in patients undergoing reoperation or those with a higher surgical invasiveness index.ii Additional risk factors include age over 65 and thoracic surgical involvement. Appropriate patient selection and planning are essential to support treatment success and minimise the potential for complications.
Benefits of Embolisation
Despite continued discussion in the field, evidence demonstrates that preoperative embolisation of carotid body tumours followed by immediate resection is associated with reduced blood loss and shorter surgical duration.iii Researchers have also found low complication rates associated with the embolisation procedure of just 3%, with success reported in the treatment of spinal tumours.iv
As the vertebral column is the most common site of bony metastasis, research continues into the optimisation of treatment techniques in the area. A systematic review confirmed that preoperative arterial embolisation of hypervascular tumours could prove beneficial in the reduction of bleeding and operative times.v
Choosing the Right Solution
In planning embolisation procedures, the selection of appropriate embolic agents plays a key role in supporting procedural efficiency and control. Equipment should be selected based on the specific clinical context and treatment goals. The Varian Embozene™ and Embozene TANDEM™ Microspheres, available through Getz Healthcare, are used in cases where targeted embolisation is indicated. Both options are precisely calibrated and available in a range of sizes to support procedural control and delivery.
To learn more about Varian Embozene™ and Embozene TANDEM™ Microspheres available from Getz Healthcare, click here.
i Nakamura H, Tanaka S, Miyanishi K, et al. A case of hypervascular tumors in the liver and pancreas: synchronous hepatocellular carcinoma and pancreatic metastasis from renal cell carcinoma 36 years after nephrectomy. Clin Case Rep. 2021; 9: 932–937. https://doi.org/10.1002/ccr3.3691
ii Tang B, Ji T, Tang X, Jin L, Dong S, Guo W. Risk factors for major complications in surgery for hypervascular spinal tumors: an analysis of 120 cases with adjuvant preoperative embolization. Eur Spine J. 2015 Oct;24(10):2201-8. doi: 10.1007/s00586-015-4122-8. Epub 2015 Jul 18. PMID: 26187620.
iii Shiga K, Katagiri K, Ikeda A, Saito D, Oikawa SI, Tsuchida K, Miyaguchi J, Kusaka T, Tamura A. Challenges of Surgical Resection of Carotid Body Tumors - Multiple Feeding Arteries and Preoperative Embolization. Anticancer Res. 2022 Feb;42(2):645-652. doi: 10.21873/anticanres.15522. PMID: 35093862.
iv Binh NT, Hoa TQ, Linh LT, My TT, Anh PQ, Duc NM. Preoperative embolization of hypervascular spinal tumors: Two case reports. J Clin Imaging Sci. 2022 May 2;12:21. doi: 10.25259/JCIS_20_2022. PMID: 35673594; PMCID: PMC9168289.
v Al-Mistarehi AH, Slika H, El Baba B, Sattari SA, Weber-Levine C, Jiang K, Lee SH, Redmond KJ, Theodore N, Lubelski D. Optimizing surgical strategies: a systematic review of the effectiveness of preoperative arterial embolization for hyper vascular metastatic spinal tumors. Spine J. 2025 Jan 13:S1529-9430(25)00017-8. doi: 10.1016/j.spinee.2024.12.032. Epub ahead of print. PMID: 39814208.
Disclaimer:
The content of this blog is intended for informational purposes only and should not be considered medical advice. Healthcare professionals should always be consulted for personalised medical guidance before pursuing any diagnosis, treatment, or medical procedure.
Getz Healthcare is proud to be recognized as the leading distributor of medical equipment, devices and consumables, in Asia Pacific.
Our full-service distribution capabilities provide end-to-end representation of our business partners’ products, while delivering comprehensive service and solutions to our customers in all the countries we serve. Learn more
All product information listed on this site are for healthcare professionals only. Descriptions and specifications of the products listed on this site are provided by the manufacturer.